Lecture on Physiology of the Heart
The heart is a powerful, rhythmic pump designed to maintain continuous blood flow throughout the body. Its physiology involves multiple interacting systems: electrical conduction, mechanical contraction, blood flow regulation, pressure control, and energy metabolism. To understand cardiac physiology deeply, we must examine each step from impulse generation to blood ejection.
Anatomical foundation for physiology
The heart is composed of three major layers: endocardium, myocardium and epicardium. The myocardium plays the primary role in contraction because it contains specialized cardiac muscle cells known as cardiomyocytes. These cells are unique as they function involuntarily and have intercalated discs that allow rapid electrical spread. These discs contain gap junctions, which act like open gates allowing ions to move quickly between cells, enabling the heart to contract as a single coordinated unit known as a functional syncytium. This property is the basis for synchronized heartbeat.
The cardiac cycle in depth
Each heartbeat has two major phases, systole and diastole.
Diastole begins when ventricles relax and their internal pressure drops. This pressure drop causes the AV valves (mitral and tricuspid) to open, allowing blood to flow passively from the atria into ventricles. This passive filling contributes nearly 70 percent of ventricular filling. Towards the end of diastole, the atria contract and push the remaining 30 percent of blood into ventricles; this is known as atrial kick. Clinically, loss of atrial kick, as seen in atrial fibrillation, reduces cardiac output.
Systole begins when the ventricles contract, causing a sharp rise in ventricular pressure. When this pressure becomes greater than atrial pressure, the AV valves close, producing the first heart sound. As contraction continues, when ventricular pressure exceeds arterial pressure, semilunar valves open and blood is ejected. This ejection has two parts: rapid ejection when blood flows quickly, and reduced ejection as the pressure gradient decreases. Ventricular relaxation begins afterward, forming isovolumetric relaxation where all valves close, allowing ventricular pressure to fall.
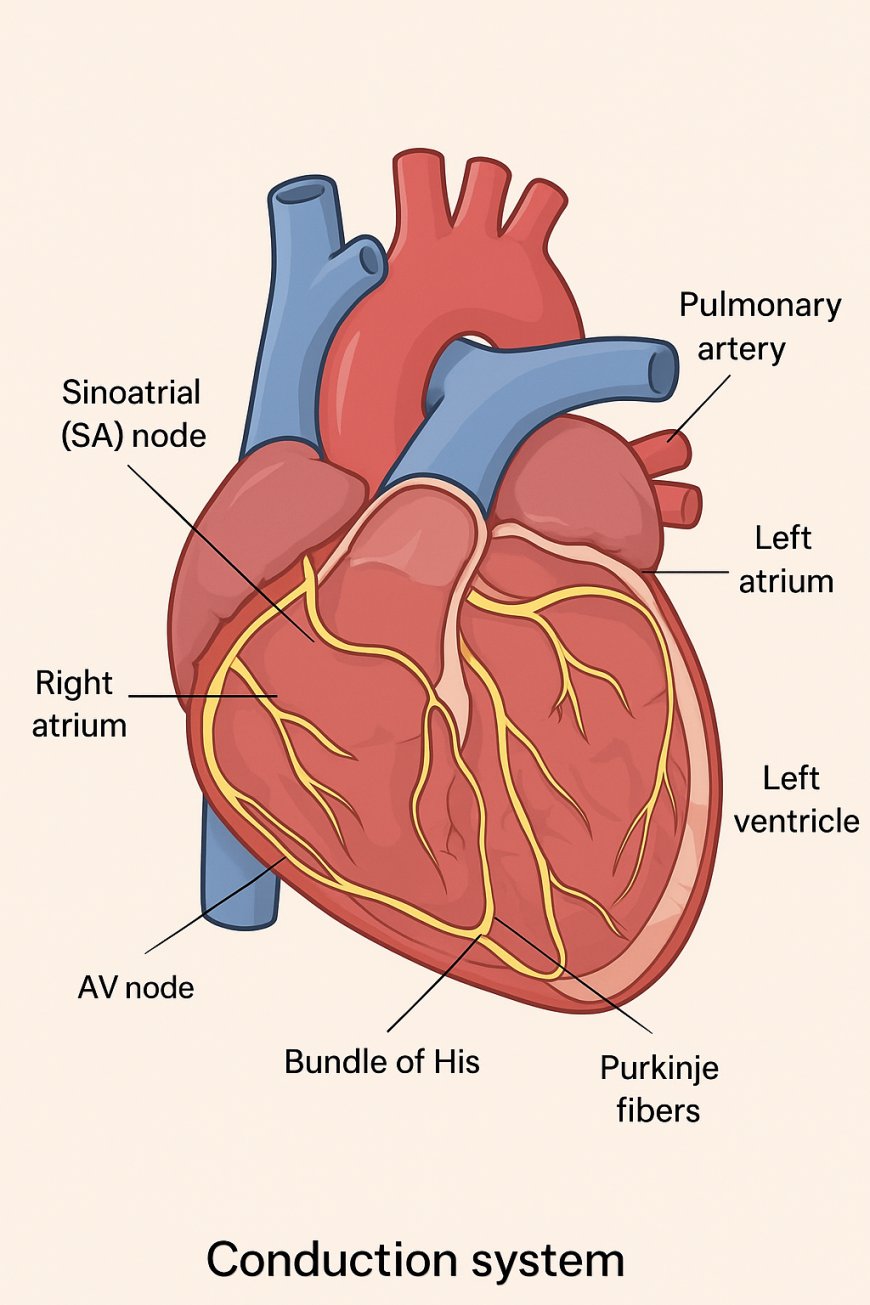
Electrical conduction in deeper detail
The conduction system ensures that all parts of the heart contract in proper order. The SA node has inherent automaticity due to unstable resting membrane potential. It gradually depolarizes because of slow inward sodium (funny current) and calcium channels. When threshold is reached, an action potential fires. This mechanism creates spontaneous rhythmic impulses without nerve input.
The impulse spreads through atrial muscle until it reaches the AV node. The AV node conducts impulses slowly because it contains fewer gap junctions. This delay is crucial because it allows ventricles enough time to fill before contraction starts. Without this delay, blood would not move efficiently.
From the AV node, the signal passes through the bundle of His, the right and left bundle branches and finally to the Purkinje fibers. Purkinje fibers transmit impulses extremely rapidly due to their large diameter and abundant gap junctions. This fast transmission ensures rapid and coordinated ventricular contraction from the apex upwards.
Cardiac action potential differences
Cardiac muscles have unique action potentials with five phases.
Phase 4 is resting membrane potential.
Phase 0 is rapid depolarization due to sodium influx.
Phase 1 is brief repolarization.
Phase 2 is the plateau phase where calcium influx balances potassium efflux. The plateau is vital because it prolongs contraction, preventing tetany.
Phase 3 is repolarization where potassium efflux dominates.
This prolonged action potential explains why the heart cannot sustain continuous contraction and must beat rhythmically.
Regulation of heart rate and contractility
Heart rate is primarily controlled by the autonomic nervous system. Sympathetic stimulation increases heart rate by enhancing slope of phase 4 depolarization in SA node. Parasympathetic stimulation through vagus nerve decreases heart rate by slowing depolarization. Contractility is increased by sympathetic activation through increased calcium availability inside muscle cells. Increased calcium means stronger contraction. Conditions like hyperthyroidism also increase contractility. Conversely, heart failure decreases contractility.
Cardiac output regulation in detail
Cardiac output equals heart rate multiplied by stroke volume. Stroke volume is affected by preload, afterload and contractility.
Preload is influenced by venous return. Increased venous return stretches myocardial fibers, enhancing contraction via Frank–Starling mechanism. This is similar to stretching a spring; more stretch produces stronger recoil.
Afterload represents the resistance the ventricles must overcome. Higher afterload, like hypertension, reduces stroke volume because the heart must work harder.
Contractility depends on calcium handling. Drugs such as digitalis increase contractility, while low oxygen reduces it.
Pressure and volume relationship
The left ventricle undergoes predictable pressure changes during each cycle. The pressure-volume loop is an advanced concept that shows how ventricular volume changes with pressure. It demonstrates isovolumetric contraction, ejection, isovolumetric relaxation and filling. Any shift in this loop indicates abnormalities such as heart failure, valve stenosis or hypertension.
Coronary circulation importance
The heart receives its own blood supply from the coronary arteries. Most coronary perfusion occurs during diastole because systole compresses the coronary vessels. Conditions like tachycardia reduce diastolic time and decrease coronary perfusion, leading to ischemia. This is why angina often occurs during exertion.
Coronary arteries supply specific regions of the heart. The left anterior descending artery supplies the interventricular septum and anterior wall. Blockage here causes severe infarction and is clinically known as the widow-maker.
Metabolism and oxygen demand
Heart muscle primarily uses aerobic metabolism. It relies heavily on oxygen and has a high concentration of mitochondria. Even brief interruptions in blood supply cause chest pain and cell injury. During exercise or stress, increased sympathetic activity increases oxygen demand.
Heart sounds and valve physiology
The first heart sound occurs when AV valves close. The second sound occurs when semilunar valves close. Additional sounds such as S3 and S4 indicate abnormal filling. Murmurs arise when valves become stenotic or regurgitant. For example, mitral stenosis causes a diastolic murmur because blood struggles to flow from left atrium to ventricle.
Clinical examples for clarity
In ventricular hypertrophy, muscle fibers become thick due to chronic pressure load. This increases oxygen demand and reduces chamber size.
In heart failure, contractility decreases, leading to reduced cardiac output. Body compensates by increasing heart rate and retaining fluid.
In complete heart block, SA node fires normally but impulses do not reach ventricles. Ventricles create their own slow rhythm which is insufficient, so a pacemaker is required.
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0