Care of poisoning patient
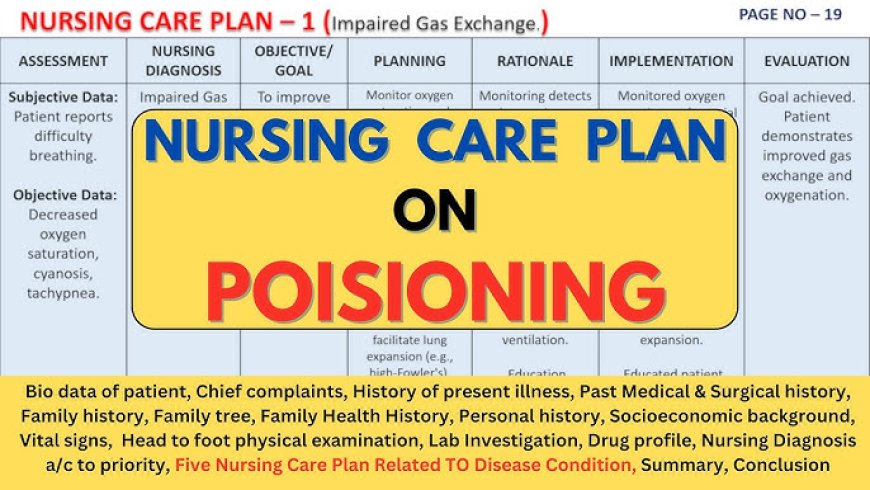
Care of poisoning patient
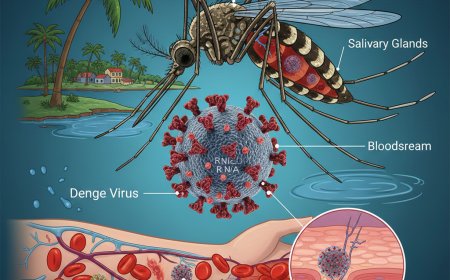
Poisoning can occur through various routes—by ingestion (swallowing), inhalation (breathing in gases or fumes), injection (through needles or bites), or absorption (through skin contact). The type and severity of poisoning depend on the nature of the substance, the dose, the route of entry, and the time elapsed since exposure. In all cases, early recognition and prompt first aid are critical before the patient reaches professional medical care.
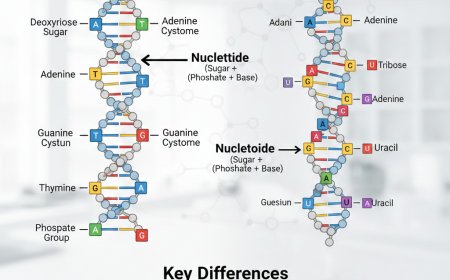
Definition and Causes (Where “Definition” and “Classification” points are explained)
In simple terms, poisoning is the entry of a toxic substance into the body that disrupts normal physiological functions or damages body tissues. Poisons may include household chemicals like detergents, medicines taken in overdose, pesticides, alcohol, industrial fumes, or venom from bites and stings. The causes can vary—from accidental ingestion by children, self-harm attempts, occupational exposure, or food contamination.
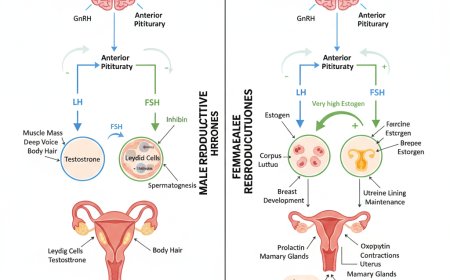
The routes of poisoning are often emphasized in first aid training. For example, ingested poisons include drugs or chemicals swallowed by mouth; inhaled poisons involve gases such as carbon monoxide or smoke; injected poisons may include drug overdoses or animal venom; and absorbed poisons result from contact with toxic substances through the skin.
Signs and Symptom
Recognizing the signs and symptoms of poisoning helps guide immediate care. Common signs include nausea, vomiting, abdominal pain, difficulty breathing, confusion, seizures, or loss of consciousness. Specific indicators may also point to the type of poison—for instance, burns around the mouth may suggest corrosive ingestion, while an unusual smell on the breath may indicate alcohol or pesticide poisoning. Pinpoint pupils are seen in opioid poisoning, whereas dilated pupils may occur in anticholinergic poisoning.
First Aid Principles
When giving first aid to a poisoning patient, the first principle is safety—for both the rescuer and the victim. The rescuer must ensure that the environment is safe before approaching the patient. Avoid touching, inhaling, or tasting the suspected poison. In the case of gas leaks or fumes, open windows and doors, and remove the patient to a well-ventilated area.
Next, follow the ABC rule—Airway, Breathing, and Circulation. Check that the airway is clear; remove any vomit or obstruction. Assess whether the patient is breathing normally and has a pulse. If the patient is not breathing, start CPR immediately if trained to do so. Once the patient’s vital functions are stabilized, call for emergency medical assistance or contact the local poison control center. Provide clear details such as what substance was taken, how much, when, and what symptoms are present.
Preventing Further Absorption
The next goal is to prevent further absorption of the poison. The approach depends on the route of poisoning.
If the poison has been ingested, do not induce vomiting unless advised by a medical professional, as this can cause further injury—especially with corrosives like acids or petroleum products. If the person is conscious, give small sips of water or milk to dilute the poison.
For inhaled poisons, move the patient immediately into fresh air and loosen tight clothing.
For absorbed poisons, such as chemical spills on the skin, remove contaminated clothing and wash the affected area with plenty of running water for at least 15–20 minutes.
In injected poisons such as snake bites or insect stings, keep the affected limb immobilized and below heart level. Do not cut, suck, or tightly tie the area, as these can worsen tissue damage.
Supportive Care
While waiting for professional help, the first aider should continue supporting vital functions. Keep the patient warm and comfortable, and if the patient is unconscious but breathing, place them in the recovery position—on their side with the head tilted back to maintain an open airway and prevent aspiration of vomit. Oxygen may be administered if available and the rescuer is trained to use it. Monitor breathing, pulse, and level of consciousness continuously until medical help arrives.
Evidence Preservation
Collecting and preserving evidence is an often-overlooked but essential step. Any bottles, containers, labels, or remnants of the suspected poison should be taken to the hospital. If the patient has vomited, a small sample can be kept in a clean container for laboratory analysis. These materials can help healthcare providers identify the poison and decide on appropriate treatment. Note the time, route, and approximate quantity of poison exposure if known.
Antidotes and Hospital Care
In hospital settings, doctors may use specific antidotes to counteract certain poisons. For instance, naloxone is the antidote for opioid poisoning, atropine and pralidoxime for organophosphate poisoning, N-acetylcysteine for paracetamol overdose, and chelating agents like EDTA for heavy metal poisoning. However, these should never be administered outside a medical facility without professional guidance, as wrong treatment can worsen the situation.
Prevention
The best way to deal with poisoning is prevention. All medicines, chemicals, and cleaning agents should be stored in labeled, childproof containers and kept out of children’s reach. Individuals should never take medication not prescribed for them, and dosing instructions must always be followed. Workers handling pesticides or chemicals should use protective clothing and ensure proper ventilation. Community education about the dangers of household and agricultural poisons can significantly reduce poisoning incidents.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0