Lecture: on Female Reproductive System – Anatomy, Physiology, and Glandular Functions
🌸 Lecture: The Female Reproductive System – Anatomy, Physiology, and Glandular Functions
Introduction
The female reproductive system is a complex and finely tuned biological system responsible for producing female gametes (ova), housing and nourishing a developing fetus, and producing female sex hormones. Its functions are cyclical, culminating in either menstruation or pregnancy.
Part 1: Anatomy of the Female Reproductive System
The female reproductive system can be divided into external and internal organs.
A. External Genitalia (Vulva)
These structures protect the internal organs and play a role in sexual arousal.
-
Mons Pubis: A fatty, rounded area overlying the pubic symphysis, covered with hair after puberty.
-
Labia Majora: Two prominent folds of skin extending from the mons pubis, enclosing the other external structures. They are homologous to the male scrotum.
-
Labia Minora: Two smaller, hairless folds of skin located medial to the labia majora. They protect the vaginal and urethral openings.
-
Clitoris: A small, highly sensitive erectile organ homologous to the male penis. It is a key organ in female sexual arousal, containing abundant nerve endings.
-
Vestibule: The space between the labia minora, containing the openings of the urethra, vagina, and the ducts of the greater vestibular glands.
-
Perineum: The diamond-shaped region between the thighs, containing the external genitalia and anus.
B. Internal Genitalia
These organs are located within the pelvic cavity and are crucial for reproduction.
-
Ovaries (Paired Gonads): Almond-shaped organs located on either side of the uterus. They are the primary female reproductive organs with dual functions:
-
Oogenesis: Production of female gametes (ova).
-
Endocrine: Production of female sex hormones, primarily estrogen and progesterone.
-
-
Uterine Tubes (Fallopian Tubes or Oviducts): Tubes extending from the uterus towards the ovaries, but not directly connected to them. They are the usual site of fertilization. Each tube has distinct regions:
-
Infundibulum: The funnel-shaped distal end, fringed with finger-like projections called fimbriae that sweep the ovum into the tube.
-
Ampulla: The widest and longest part, where fertilization most commonly occurs.
-
Isthmus: The narrower, medial portion joining the uterus.
-
-
Uterus (Womb): A hollow, thick-walled, muscular organ located between the bladder and the rectum. Its primary functions are to receive, retain, and nourish a fertilized ovum. It has several regions:
-
Fundus: The rounded superior portion above the entrance of the uterine tubes.
-
Body (Corpus): The major portion of the uterus.
-
Cervix: The narrow, inferior neck that projects into the vagina.
The uterine wall has three layers:
-
Perimetrium: Outermost serous layer.
-
Myometrium: Thick middle layer of smooth muscle, responsible for contractions during childbirth.
-
Endometrium: Innermost mucosal layer, which is shed during menstruation if pregnancy does not occur. It consists of a functional layer (stratum functionalis) and a basal layer (stratum basalis).
-
-
Vagina: A muscular tube extending from the cervix to the exterior of the body. It serves as:
-
The female organ of copulation.
-
The birth canal.
-
The passageway for menstrual flow.
-
Part 2: Physiology of the Female Reproductive System
The physiology revolves around two interconnected cycles: the Ovarian Cycle (changes in the ovary) and the Uterine Cycle (changes in the uterus). These are tightly regulated by hormones.
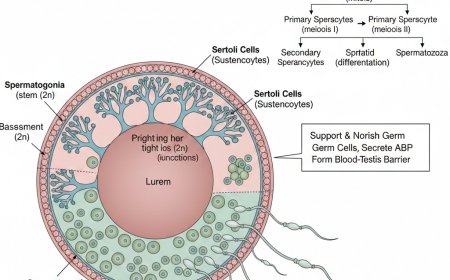
A. Oogenesis: Ovum Production
Oogenesis is the process of egg cell formation, occurring in the ovaries.
-
Fetal Development: Oogonia (diploid stem cells) undergo mitosis to produce primary oocytes. These begin meiosis I but arrest in prophase I until puberty. A female is born with her lifetime supply of primary oocytes (around 1-2 million).
-
From Puberty to Menopause: Each month, a few primary oocytes are stimulated to complete meiosis I, forming a large secondary oocyte and a small first polar body. The secondary oocyte then arrests in metaphase II and is ovulated.
-
Fertilization: If a sperm penetrates the secondary oocyte, it quickly completes meiosis II, forming a large ovum (egg) and a small second polar body.
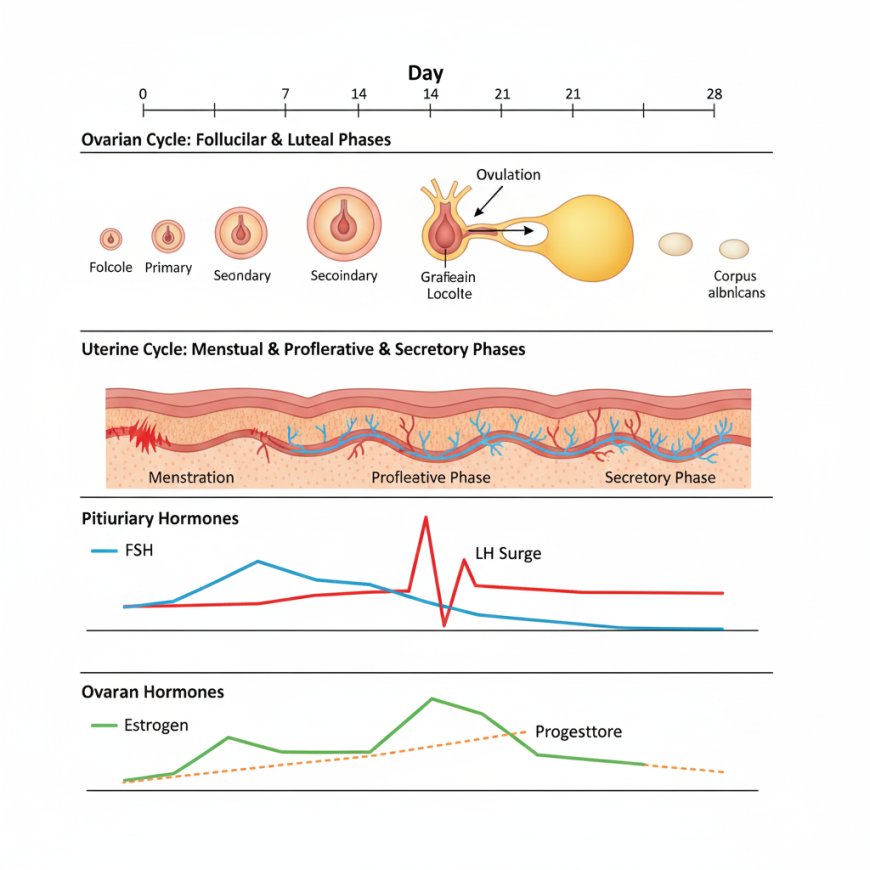
B. The Ovarian Cycle
This describes the monthly events in the ovaries that lead to ovulation. It has three phases:
-
Follicular Phase (Day 1-14):
-
Primordial follicles (primary oocyte surrounded by a single layer of flat follicle cells) are stimulated to develop.
-
They grow into primary, secondary, and finally a mature Graafian (vesicular) follicle.
-
Granulosa cells of the developing follicle produce estrogen.
-
The dominant follicle secretes a large amount of estrogen, leading to an LH surge.
-
-
Ovulation (Around Day 14):
-
The LH surge triggers the rupture of the Graafian follicle, expelling the secondary oocyte into the peritoneal cavity (where it is swept into the uterine tube).
-
-
Luteal Phase (Day 14-28):
-
The ruptured follicle transforms into the Corpus Luteum under the influence of LH.
-
The corpus luteum secretes large amounts of progesterone and some estrogen.
-
If no pregnancy occurs, the corpus luteum degenerates into a corpus albicans after about 10 days, leading to a drop in hormone levels and menstruation.
-
If pregnancy occurs, the corpus luteum persists, maintained by hCG (human chorionic gonadotropin) from the embryo, continuing to produce hormones until the placenta takes over.
-
C. The Uterine (Menstrual) Cycle
This describes the cyclical changes in the endometrial lining of the uterus, responding to ovarian hormones. It also has three phases:
-
Menstrual Phase (Days 1-5):
-
Triggered by the drop in ovarian hormones (estrogen and progesterone) as the corpus luteum degenerates.
-
The stratum functionalis of the endometrium detaches from the uterine wall, causing bleeding (menstruation).
-
-
Proliferative Phase (Days 6-14):
-
Rising estrogen levels from the developing ovarian follicles stimulate the regeneration and thickening of the stratum functionalis.
-
Endometrial glands enlarge, and spiral arteries increase in number.
-
-
Secretory Phase (Days 15-28):
-
Rising progesterone levels from the corpus luteum prepare the endometrium for implantation.
-
Endometrial glands secrete nutrients (glycogen), and the spiral arteries become highly coiled and elaborate.
-
If fertilization and implantation occur, the embryo will implant into this highly vascularized and nutrient-rich endometrium.
-
If no pregnancy, progesterone levels drop, causing vasoconstriction of the spiral arteries, leading to cell death and the start of the next menstrual phase.
-
Part 3: Hormonal Regulation (The HPG Axis)
The female reproductive cycle is exquisitely controlled by the Hypothalamic-Pituitary-Gonadal (HPG) axis and local ovarian factors.
-
Hypothalamus: Releases Gonadotropin-Releasing Hormone (GnRH) in a pulsatile fashion.
-
Anterior Pituitary: GnRH stimulates the release of two gonadotropins:
-
Follicle-Stimulating Hormone (FSH): Stimulates follicle growth and estrogen production by granulosa cells.
-
Luteinizing Hormone (LH): Triggers ovulation and promotes the formation and maintenance of the corpus luteum (and thus progesterone production).
-
-
Ovaries (Gonads):
-
Estrogen: Produced primarily by developing follicles. Responsible for:
-
Promoting oogenesis and follicle growth.
-
Developing and maintaining female secondary sexual characteristics.
-
Stimulating proliferation of the endometrium.
-
Inhibiting FSH and LH release (negative feedback) at low levels, but causing a massive surge of LH (positive feedback) at high, sustained levels just before ovulation.
-
-
Progesterone: Produced primarily by the corpus luteum. Responsible for:
-
Maintaining the secretory endometrium, preparing it for implantation.
-
Inhibiting uterine motility.
-
Exerting negative feedback on the hypothalamus (GnRH) and anterior pituitary (LH and FSH), preventing further follicle development and ovulation during the luteal phase and pregnancy.
-
-
Inhibin: Produced by granulosa cells and the corpus luteum. Selectively inhibits FSH release from the anterior pituitary.
-
Part 4: Female Glands and Their Functions
Beyond the ovaries, several other glands play supportive roles.
-
Greater Vestibular Glands (Bartholin's Glands):
-
Location: Pea-sized glands located on either side of the vaginal opening.
-
Function: Secrete mucus into the vestibule during sexual arousal, providing lubrication for intercourse.
-
-
Lesser Vestibular Glands (Skene's Glands or Paraurethral Glands):
-
Location: Located on either side of the urethral opening.
-
Function: Secrete mucus to lubricate the opening of the urethra and vestibule. Some researchers believe these glands may be homologous to the male prostate gland and contribute to "female ejaculation."
-
-
Mammary Glands (Breasts):
-
Location: Modified sweat glands located in the superficial fascia of the anterior thorax.
-
Structure: Consist of 15-25 lobes, which contain smaller lobules with alveoli (milk-producing glands). The milk drains via lactiferous ducts which open at the nipple.
-
Function: Produce milk (lactation) to nourish an infant after childbirth.
-
Estrogen and progesterone stimulate breast development during puberty and pregnancy.
-
Prolactin (from the anterior pituitary) stimulates milk production.
-
Oxytocin (from the posterior pituitary) stimulates milk ejection (let-down reflex) in response to suckling.
-
-
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0