Anatomy of the Male Reproductive System
Anatomy of the Male Reproductive System (Basic)
The male reproductive system is designed to produce, maintain, and transport sperm (male reproductive cells) and protective fluid (semen) and to discharge sperm within the female reproductive tract.
External Organs
-
Penis: The male organ for sexual intercourse and urination. It contains three chambers of specialized erectile tissue: two large corpora cavernosa and one corpus spongiosum (which surrounds the urethra). Erection occurs when these chambers fill with blood.
-
Scrotum: A loose pouch-like sac of skin hanging behind the penis. Its primary function is temperature regulation (the testes must be slightly cooler than body temperature, around $36^\circ \text{C}$ or $97-99^\circ \text{F}$), which is vital for normal sperm development.
-
Testes (Testicles): Oval-shaped organs housed in the scrotum. They are the primary male reproductive organs (gonads) and have dual functions:
-
Exocrine: Production of sperm.
-
Endocrine: Production of the primary male sex hormone, testosterone.
-
-
Epididymis: A long, coiled tube resting on the back of each testis. It transports and stores sperm and is the site where sperm mature and gain the ability to move (motility) and fertilize.
Internal Ducts and Accessory Glands
The internal system is responsible for sperm maturation, transport, and the production of semen.
-
Vas Deferens (Ductus Deferens): A long, muscular tube that transports mature sperm from the epididymis to the ejaculatory duct during sexual arousal.
-
Accessory Glands: These glands produce the fluid portion of semen (seminal plasma), which nourishes and protects the sperm.
-
Seminal Vesicles (paired): Sac-like glands posterior to the bladder. They contribute about 60% of the semen volume. The fluid is viscous and rich in fructose (energy for sperm) and prostaglandins (thought to aid sperm transport).
-
Prostate Gland: A walnut-sized gland inferior to the bladder, encircling the urethra. Its secretions are thin, milky, and slightly alkaline, which helps neutralize the acidity of the female reproductive tract and enhances sperm motility.
-
Bulbourethral Glands (Cowper's Glands, paired): Small glands near the base of the penis. They secrete an alkaline mucus-like fluid just prior to ejaculation (pre-ejaculate) to lubricate the urethra and neutralize any residual urine acidity.
-
-
Urethra: The tube that passes through the penis and serves as the exit pathway for both urine and semen.
🔬 Physiology: Production, Regulation, and Ejaculation (Advanced)
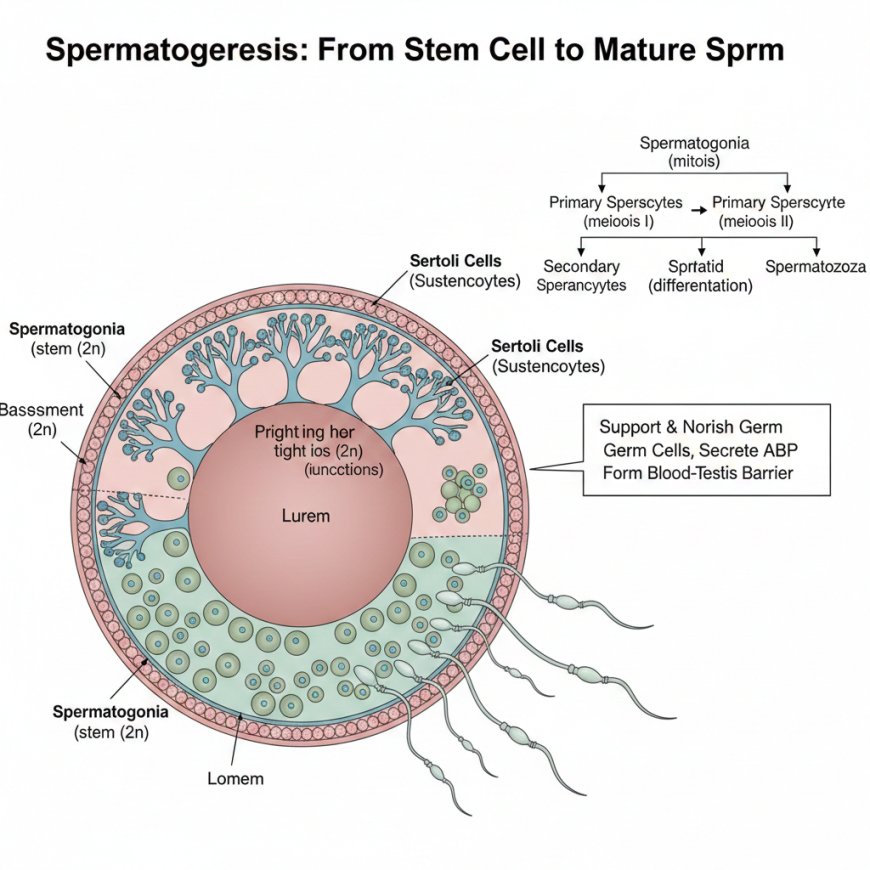
1. Spermatogenesis: Sperm Production
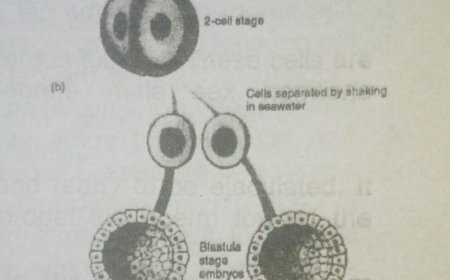
Spermatogenesis is the process of sperm cell production, occurring within the tightly coiled seminiferous tubules inside the testes. This process takes approximately 64-72 days and begins at puberty.
| Cell Type | Location/Support | Role/Significance |
| Spermatogonia | Lining the basement membrane of the seminiferous tubules | Diploid stem cells that undergo mitosis to replenish themselves and produce primary spermatocytes. |
| Spermatocytes/Spermatids | Inside the seminiferous tubules | Primary spermatocytes undergo meiosis I to become secondary spermatocytes (haploid), which then undergo meiosis II to become spermatids (haploid). |
| Sertoli Cells (Sustenocytes) | Within the seminiferous tubules | Support cells for the developing germ cells. They secrete signaling molecules, nutrients, and the Androgen-Binding Protein (ABP). They also form tight junctions creating the Blood-Testis Barrier (BTB), which protects developing sperm from the immune system. |
| Spermatozoa (Sperm) | Released into the lumen of the tubules | Mature male gametes. Consist of a head (contains the haploid nucleus and an acrosome cap with enzymes for fertilization), a midpiece (packed with mitochondria for energy), and a tail/flagellum (for motility). |
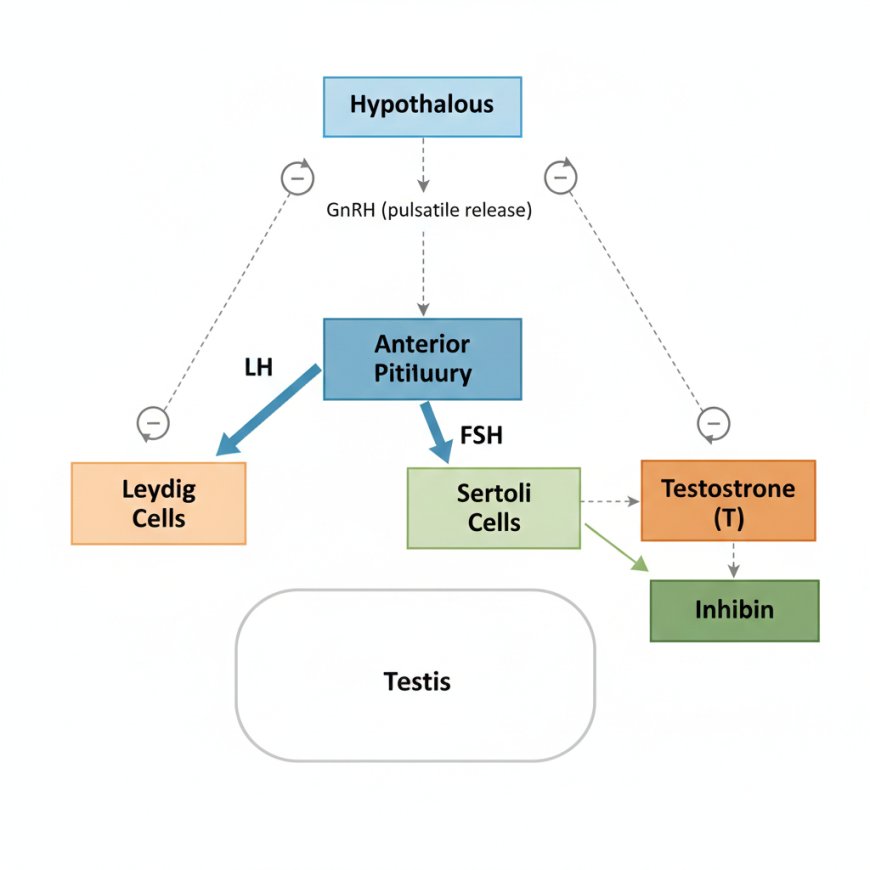
2. Hormonal Regulation (The HPG Axis)
he function of the testes is regulated by the Hypothalamic-Pituitary-Gonadal (HPG) axis via a negative feedback loop.
-
Hypothalamus: Releases Gonadotropin-Releasing Hormone (GnRH) in pulses.
-
Anterior Pituitary: GnRH stimulates the release of two gonadotropins:
-
Luteinizing Hormone (LH): Stimulates the Leydig cells (found in the interstitium between the tubules) to produce Testosterone.
-
Follicle-Stimulating Hormone (FSH): Acts on the Sertoli cells to promote spermatogenesis and secrete ABP.
-
-
Testes (Gonads):
-
Testosterone (T): Essential for spermatogenesis (acting via Sertoli cells) and for developing/maintaining male secondary sexual characteristics. T exerts negative feedback on both the hypothalamus (GnRH) and the anterior pituitary (LH and FSH).
-
Inhibin: Produced by Sertoli cells. Selectively provides negative feedback to the anterior pituitary to inhibit FSH secretion.
-
3. Advanced Physiology: Erection and Ejaculation
Erection
Erection is primarily a parasympathetic nervous system response, facilitated by the release of nitric oxide (NO).
-
NO relaxes the smooth muscle walls of the arteries in the corpora cavernosa and corpus spongiosum, allowing blood to flow in and engorge the erectile tissue.
-
The expanding erectile tissue compresses the veins (venous occlusion), trapping the blood and maintaining the erection.
-
Phosphodiesterase-5 (PDE5) is an enzyme that degrades the molecules that cause this smooth muscle relaxation, leading to detumescence (loss of erection).
Ejaculation
Ejaculation is a two-phase reflex event involving both sympathetic and somatic nervous systems.
-
Emission (Sympathetic): Smooth muscle contractions in the walls of the epididymis, vas deferens, seminal vesicles, and prostate move sperm and seminal fluid into the urethra (internal sphincter of the bladder also contracts to prevent retrograde ejaculation).
-
Expulsion (Somatic/Sympathetic): Rhythmic contractions of the skeletal muscles at the base of the penis (bulbospongiosus muscle) propel the semen out through the urethra.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0