Short Conceptual Questions (20)
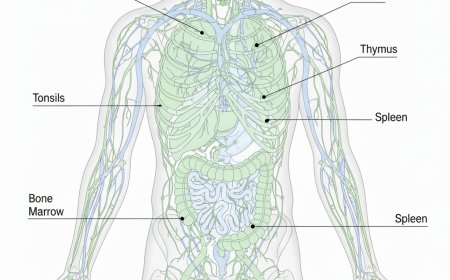
1. Trace the functional role of lymph during interstitial–vascular fluid shifts.
Ans:Trace the functional role of lymph during interstitial–vascular fluid shifts
Lymph acts as the recovery pathway for excess fluid that escapes from blood capillaries into the interstitial spaces.When hydrostatic pressure pushes fluid out of vessels, lymphatic capillaries absorb the surplus to prevent tissue swelling.This absorbed fluid carries proteins, metabolic waste, and immune cells back toward the circulation.
One-way valves in lymphatic vessels keep the movement directed toward the venous system. Muscle contractions and vessel wall pulsations help propel lymph forward during body movement. By continuously returning lost fluid and proteins, the lymphatic system maintains circulating blood volume and prevents edema.
2. Highlight the immune-filtering behavior shown by lymph nodes during pathogen entry.
Ans :Highlight the immune-filtering behavior shown by lymph nodes during pathogen entry
Lymph nodes act as biological checkpoints where incoming lymph is slowed and screened. As lymph enters through afferent vessels, it passes through a maze-like network of sinuses that trap microbes and foreign particles. Resident macrophages engulf these trapped pathogens through phagocytic activity. Dendritic cells within the node present captured antigens to lymphocytes, initiating immune activation.
B and T cells become stimulated and begin forming targeted immune responses against the identified pathogen. Cleaned lymph then exits through efferent vessels, ensuring only filtered, immune-monitored fluid returns to the bloodstream.
3. Relate cerebrospinal fluid pressure changes with altered neuronal signaling.
Ans:Relate cerebrospinal fluid pressure changes with altered neuronal signaling Cerebrospinal fluid (CSF) helps maintain a stable pressure environment around the brain and spinal cord.
When CSF pressure rises, it compresses neural tissues, which disrupts normal electrochemical signaling pathways.This compression can slow axonal conduction, alter synaptic transmission, and reduce cerebral blood flow.Low CSF pressure, on the other hand, causes brain sagging that stretches pain-sensitive structures and disturbs neural connectivity.
Both increased and decreased pressure shift the balance of ion exchange around neurons.These changes collectively lead to headaches, sensory disturbances, and impaired cognitive or motor functions.
4. Connect CSF circulation blockage with ventricular dilation patterns.
Ans :Connect CSF circulation blockage with ventricular dilation patterns
CSF normally flows from the ventricles through narrow channels and around the brain and spinal cord.When a blockage occurs, CSF continues to be produced but cannot pass beyond the obstructed site.
This trapped fluid builds pressure inside the ventricles, gradually expanding their walls.The dilation reflects the resistance created by the obstruction, causing upstream ventricles to enlarge more prominently.
Stretched ventricular walls compress surrounding brain tissue and interfere with neural pathways.Sustained dilation ultimately leads to symptoms of hydrocephalus, including pressure-related neurological deficits.
5. Examine synovial fluid viscosity variation during joint loading cycles.
Ans:Examine synovial fluid viscosity variation during joint loading cycles Synovial fluid shows a property called *thixotropy*, meaning its viscosity changes with movement and pressure.
During rapid or heavy joint loading, the fluid becomes thinner, allowing smoother motion and reducing friction between cartilage surfaces. When the joint is at rest, the fluid becomes thicker again, forming a protective cushioning layer.This variation helps distribute mechanical stress evenly across the joint.Thinner fluid during activity enhances lubrication, while thicker fluid at rest supports shock absorption.
These shifts in viscosity preserve joint integrity and minimize wear on articular cartilage.
6. Associate reduced synovial secretion with friction-induced cartilage stress.
Ans:Associate reduced synovial secretion with friction-induced cartilage stress
Synovial fluid provides essential lubrication that prevents direct rubbing of articular cartilage surfaces. When synovial secretion decreases, the joint loses its smooth, low-friction interface.
Cartilage surfaces begin to experience increased mechanical resistance during movement. This added friction accelerates micro-damage within the cartilage matrix.
Reduced lubrication also limits nutrient diffusion to the avascular cartilage, weakening its resilience.Over time, these combined stresses contribute to cartilage thinning, surface roughening, and early degenerative joint changes.
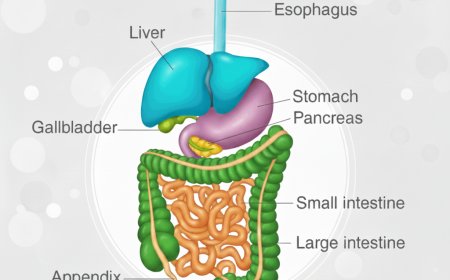
7. Outline gastric juice activity during protein denaturation phases.
Ans:Gastric juice initiates protein denaturation mainly through its acidic component, hydrochloric acid (HCl).The low pH disrupts hydrogen bonds and unfolds complex protein structures into linear chains.
This denaturation exposes peptide linkages, making them accessible for enzymatic attack.Pepsinogen, released from chief cells, is activated into pepsin in the acidic environment.
Active pepsin begins hydrolyzing the exposed peptide bonds into smaller polypeptides. Mucus in gastric juice protects the stomach lining while allowing acid–enzyme action on proteins.
Overall, gastric juice creates an optimal acidic and enzymatic phase for efficient protein breakdown.
8. Discuss the interplay of gastric acidity with intrinsic factor release.
Ans: Discuss the interplay of gastric acidity with intrinsic factor release
Gastric acidity is primarily generated by parietal cells, which also produce intrinsic factor. A strongly acidic environment stimulates these cells, promoting simultaneous secretion of both hydrochloric acid and intrinsic factor.Acid helps release vitamin B₁₂ from food proteins in the stomach. Once freed, vitamin B₁₂ can bind with intrinsic factor to form a stable complex.
This complex is essential for safe passage through the intestine without degradation.Through this coordinated relationship, gastric acidity enables intrinsic factor to perform its vital role in vitamin B₁₂ absorption.
9. Link pancreatic digestive enzymes with nutrient-specific breakdown pathways.
Ans:Link pancreatic digestive enzymes with nutrient-specific breakdown pathways
The pancreas secretes enzymes tailored to specific macronutrients into the small intestine. Amylase breaks down starches into simple sugars like maltose and glucose.
Lipase targets triglycerides, splitting them into fatty acids and glycerol for absorption. Proteases such as trypsin and chymotrypsin cleave proteins into smaller peptides and amino acids.
Nucleases degrade nucleic acids into nucleotides for cellular use.Each enzyme acts within an optimal pH and substrate environment, ensuring precise nutrient digestion. This specialization allows efficient extraction of energy and building blocks from diverse foods.
10. Investigate gallbladder bile concentration influence on lipid emulsification.
Ans :Bile stored in the gallbladder contains bile salts, cholesterol, and phospholipids that aid lipid digestion.Concentration of bile increases during fasting as water is reabsorbed, making it more potent.
Highly concentrated bile salts are more effective at breaking large lipid droplets into tiny micelles. This emulsification increases the surface area for pancreatic lipase to act efficiently.
If bile is too dilute, lipid droplets remain larger, slowing enzymatic digestion. Optimal bile concentration ensures faster absorption of fatty acids and fat-soluble vitamins.Thus, gallbladder bile concentration directly modulates the efficiency of lipid emulsification in the small intestine.
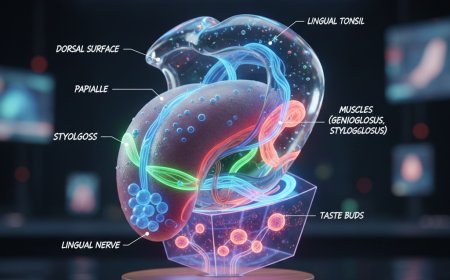
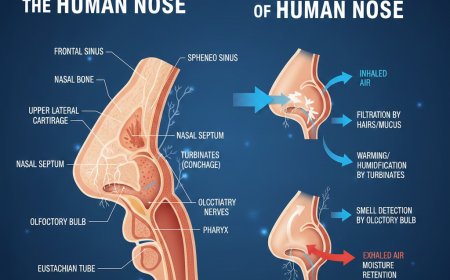
11. Integrate mucus barrier behavior with epithelial surface protection mechanisms.
Ans:Integrate mucus barrier behavior with epithelial surface protection mechanisms The mucus layer coats epithelial surfaces, forming a physical barrier against pathogens and chemical irritants.
It traps dust, microbes, and particulate matter, preventing them from reaching the underlying cells. Mucus contains antimicrobial proteins and enzymes that neutralize harmful organisms.
Hydration within the mucus supports ciliary movement in respiratory pathways, aiding clearance. By maintaining surface moisture, mucus prevents epithelial drying and mechanical damage.
it also buffers pH changes and enzymatic activity, protecting delicate tissues.Overall, mucus works synergistically with epithelial cells to preserve tissue integrity and defense.
12. Characterize mucus dehydration effects on mucociliary clearance
Dehydrated mucus becomes thicker and less mobile, impairing the cilia’s ability to move it.This slows the removal of trapped dust, pathogens, and debris from the respiratory tract.
Accumulation of viscous mucus increases infection risk and airway obstruction. Cilia may become fatigued or damaged when pushing dense mucus repeatedly.
Airway surfaces lose effective hydration, further reducing mucociliary efficiency. Persistent dehydration can lead to chronic respiratory issues like bronchitis or sinusitis. Overall, proper mucus hydration is essential for maintaining airway defense mechanisms.
13. Map lymphatic drainage disturbance to peripheral edema formation
When lymphatic drainage is impaired, interstitial fluid accumulates in tissues. The excess fluid overwhelms capillary reabsorption, causing visible swelling. Protein-rich lymph trapped in tissues increases osmotic pressure, drawing in more water. Affected areas often appear puffy and may feel heavy or tense. Prolonged stagnation can compromise local immunity and nutrient exchange.
Peripheral edema typically manifests in extremities like legs and feet first. Efficient lymphatic flow is therefore critical to prevent tissue fluid overload.-
14. Relate chylomicron transport to lymphatic vessel integrity
Chylomicrons are fat-transporting particles absorbed from the intestines. They enter lacteals, small lymphatic vessels in the villi, for transport to circulation.
Damaged or leaky lymphatic vessels hinder chylomicron movement. Impaired transport leads to fat malabsorption and nutrient deficiencies. Lymphatic vessel integrity ensures smooth delivery of dietary lipids.
Obstruction may cause localized swelling and lipid accumulation in tissues.Healthy lymphatics are essential for maintaining energy balance and fat metabolism.
15. Interpret CSF glucose shifts during meningeal inflammation
Inflammation of the meninges increases glucose consumption by invading pathogens and immune cells. This reduces glucose concentration in the cerebrospinal fluid.
Lowered CSF glucose is often detectable in diagnostic testing. Normal glucose gradients are disrupted, affecting neuronal metabolism.Neurons may experience energy shortages if CSF glucose drops significantly. Glucose shifts correlate with infection severity and disease progression. Monitoring CSF glucose helps assess meningeal inflammation impact on brain function.
16. Compare synovial membrane health with nutrient diffusion to avascular cartilage
The synovial membrane secretes fluid rich in nutrients and oxygen for cartilage.Healthy membranes ensure continuous diffusion to avascular cartilage surfaces.
Damaged membranes reduce fluid volume and nutrient supply. Cartilage becomes weaker, less resilient, and more prone to wear. Nutrient limitation accelerates degeneration and joint dysfunction.
Proper membrane function maintains joint homeostasis and mobility. Synovial health is therefore directly linked to cartilage survival and integrity.
17. Correlate gastric mucus deficiency with ulcerative lesion formation
Mucus forms a protective barrier against stomach acid and digestive enzymes. Reduced mucus exposes epithelial cells to direct acid contact.
Acid and pepsin attack the stomach lining, causing cell damage.Persistent exposure leads to erosion of tissue and ulcer formation.
Inflammatory responses exacerbate tissue breakdown.Ulcers often develop in areas with the thinnest mucus coverage.
Maintaining adequate mucus secretion is critical for gastric lining protection.
18. Study the sequence of digestive fluid release during the cephalic phase of digestion
The cephalic phase is triggered by the sight, smell, or thought of food. Neural signals stimulate the vagus nerve to activate gastric secretions.
Gastric juice, including acid and enzymes, begins to flow into the stomach. Pancreatic juice and bile are also primed for release into the duodenum. Mucus secretion increases to protect the gastric lining during initial digestion.Enzymes are distributed strategically to prepare for nutrient breakdown.This anticipatory release ensures digestion starts efficiently before food enters the stomach.
19. Evaluate gastric juice imbalance and its impact on pyloric sphincter behavior
Excessive gastric acidity can irritate the duodenal lining and trigger pyloric contraction. Low acid levels reduce pepsin activation, slowing protein digestion.
Imbalance in juice composition may cause sphincter relaxation or delayed emptying. Altered pyloric function affects gastric emptying rate and intestinal nutrient absorption.
Persistent disturbances can contribute to reflux or gastroparesis.Coordination between juice secretion and sphincter movement is essential for digestion.
Maintaining proper gastric juice balance preserves normal gastric motility and nutrient flow.
-20. Connect lymphatic vessel contraction rhythm with overall lymph propulsion efficiency Lymphatic vessels have intrinsic contractile activity that propels lymph forward.
Regular rhythmic contractions ensure steady lymph movement against gravity. rregular or weak contractions slow lymph flow, promoting fluid accumulation.
Valve function relies on contraction timing to prevent backflow.Efficient rhythm enhances immune surveillance and protein transport.Exercise and muscle activity can synchronize contractions and boost flow.
Optimal contraction rhythm is critical for maintaining fluid balance and tissue health.
Long Conceptual Questions (3)
1. Construct a detailed concept on the integrated movement of lymph from tissue spaces to the venous system, focusing on pressure gradients, lymphatic valve action, vessel contractions, and how these elements collectively maintain fluid balance and immune surveillance.
2. Develop an analytical concept linking cerebrospinal fluid formation, circulation, and absorption with neural protection, metabolic waste removal, and intracranial pressure regulation, emphasizing the consequences of disruption at any step.
3. Present a comprehensive concept describing coordinated secretions of digestive fluids—gastric juice, bile, pancreatic juice, intestinal mucus—and illustrate how their combined biochemical actions ensure digestion, lubrication, protection, and nutrient absorption within the gastrointestinal tract.
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0